
Just had Botox and itching to exercise? Hold off on that sweat session just yet. Find out exactly when and how you can safely return to your workout routine by exercising after Botox without risking your results. Our expert advice ensures you balance your fitness goals with the integrity of your Botox treatment.
Avoid strenuous exercise for 24 hours post-Botox to prevent complications like swelling or migration of the product, with some doctors advising to avoid high-impact activities for up to a week.
Recognize and manage post-Botox exercise symptoms such as pain, bruising, or redness at the injection site, and avoid hot environments, alcohol, and harsh skincare products to ensure treatment efficacy.
Use of Botox extends to managing conditions like Bell’s palsy, eye twitching, depression, muscle contractures, acne, improving scar appearance, and potentially aiding in hair rejuvenation.
Botox injections are a type of cosmetic procedure that temporarily paralyzes facial muscles to reduce the appearance of wrinkles. This botulinum toxin type A derived medication is popularly used to treat and prevent signs of aging, such as wrinkles, crow’s feet, glabellar lines, and forehead furrows. However, the post-treatment period, especially the first 24 hours, requires careful consideration of physical activities to maximize the results of the Botox work.
Vigorous exercise after Botox treatment is generally discouraged. The increase in heart rate and the increased blood flow, that accompanies strenuous exercise after Botox can cause the botox to migrate from the targeted muscles, leading to reduced effectiveness and increased chances of swelling and bruising. Consequently, it’s recommended to avoid overexerting your body and follow your doctor’s post-treatment recommendations.
Understanding which exercises are safe and which should be avoided is crucial. This not only ensures the best treatment and recovery experience but also helps maintain the refreshed and rejuvenated appearance that Botox injections aim to provide.
The question looms - when can one start exercising after Botox treatment? Well, most doctors recommend refraining from exercise for 24 hours after Botox injections to ensure optimal results. This ‘cooling-off’ period is crucial to prevent situations that could lead to complications such as bruising or migration of Botox.
This doesn’t mean you need to become a couch potato for the day. Light activities are generally safe, but anything that might increase your heart rate or increase blood flow or pressure, such as strength training, is best avoided. Not adhering to this waiting period may increase the risk of prolonged or severe swelling or bruising. Strenuous physical activities can lead to heightened blood flow and pressure in treated areas, potentially disrupting the desired effects of the Botox treatment.
While the standard advice is to wait 24 hours before resuming exercise, it’s worth noting that some doctors suggest avoiding strenuous, high-impact activities for a full week after Botox treatment. These recommendations can vary based on the specifics of the procedure and the individual’s health profile, so it’s always best to consult with a doctor or your own healthcare provider.
Once the recommended wait period is over, it’s important to gradually ease back into your fitness routine. Certain exercises are safe to perform, while others should be approached with caution.
In the following subsections, we’ll delve into the specifics of safe practices for light cardio options, strength training considerations, and flexibility and balance activities post-Botox.
Light cardio is a great way to ease back into your fitness routine after Botox. Here are some exercises you can try:
It’s important to keep blood flow and the heart rate stable without a significant increase during aerobic exercise.
Safe light cardio options, which are great for avoiding strenuous exercise, include walking, light gardening, and stationary cycling. These exercises are gentle on the body and cardiovascular system and do not disrupt the treatment area when done correctly. They offer the perfect balance, allowing you to keep active and maintain your fitness without compromising the results of your Botox treatment.
One essential point to have patients remember is to avoid bending over during these exercises. This precaution ensures that the Botox stays in the targeted muscles and doesn’t migrate to other areas, which could impact the treatment’s effectiveness.
Flexibility and balance activities, such as light yoga and stretching, are generally safe after Botox. They can help maintain muscle tone and promote relaxation without putting excessive pressure on the treated area. However, it’s important to avoid exercises that involve head bending or inversions.
For example, engaging in light yoga practices that avoid inversions and light stretching that does not involve the head bending forward or lying down is often safe. Standing balance exercises, which do not entail significant movement or changes in the position of the head, can also be safely performed following Botox treatment.
However, exercises on the floor that require bending the head or practicing downward positions, as well as inversions such as headstands or yoga poses like Downward Dog, should be avoided. These activities can cause the botox to spread from the treated area to surrounding muscles, reducing its effectiveness.
When it comes to strength training post-Botox, a little caution goes a long way. The key is to avoid exercises that compromise head positioning or put pressure on the injection site. Remember, maintaining your head upright is a key post-Botox instruction to minimize the risk of product migration.
Positions such as lying down or bending over may counteract the post-Botox care protocol. Thus, weight lifting and other strength training activities involving potentially compromising positions should be avoided within the first four hours or workout after botox treatment.
Adhering to the instruction to keep the head upright following Botox injections will contribute to the overall success and safety of the treatment. It may seem a little restrictive initially, but the results are worth the effort!

As important as it is to know which facial exercises are safe after Botox, it’s equally crucial to know which ones to avoid. Here are some exercises to avoid post-Botox:
These exercises can increase the blood pressure and flow, which may cause the Botox to migrate from the treated area, leading to reduced effectiveness and increased chances of swelling, bruising, and excessive sweating.
It’s also best to avoid:
Moreover, it is crucial to avoid exercises that could cause excessive pressure on the treatment area or require the face to strain. This could encourage the treated neurotoxin to migrate and affect results, especially within the first 24 hours after injection. Remember, following your doctor’s post-treatment instructions can go a long way in ensuring the best possible outcome for your Botox treatment.
While the benefits of Botox are substantial, it’s important to be aware of potential side effects post-treatment, especially when exercising. Temporary pain or discomfort at the injection site, along with potential bruising and redness, are immediate or early side effects that might arise from exercising post-Botox.
If you notice more serious side effects such as muscle weakness, difficulty swallowing or breathing, poor bladder control, or vision changes after exercising post-Botox, it’s crucial to seek immediate medical attention. Engaging in vigorous exercise much too soon after Botox can:
To alleviate mild post-exercise symptoms like headaches, over-the-counter pain relievers such as Tylenol can be used. To reduce swelling or bruising, it’s advised to minimize excessive movement and take it easy for the day. Always remember that while maintaining an active lifestyle post-Botox is important, it should not come at the cost of your health or the effectiveness of your treatment.
Keeping your skin happy after Botox involves more than just refraining from certain exercises. After receiving Botox, avoid hot tubs, saunas, or participating in hot yoga, as these can encourage bruising and affect treatment efficacy. Alcohol should also be avoided for 24 hours after Botox treatment to reduce the risk of bruising and to ensure the treatment’s effectiveness.
Furthermore, resume a regular skincare routine 24 hours after Botox treatment. This includes gentle cleansing, toning, and moisturizing, but avoid massaging the area or using abrasive skincare products for at least a week. High-quality skincare products with antioxidants, peptides, and hyaluronic acid are recommended post-Botox to hydrate the skin and promote cell turnover. However, skincare products containing retinol and glycolic acid should be avoided on the treated areas for at least a week following Botox to prevent irritation.
Last but not least, here are some tips to follow after getting Botox:
Always use a broad-spectrum sunscreen with an SPF of at least 30 every day to protect the skin. Excessive sun exposure can diminish the effects of the treatment and should be avoided for 24-48 hours post-procedure.
Manage your dietary intake by avoiding salty or processed foods post-Botox to help reduce swelling.
Include fruits like pineapple in your diet, as they may help prevent bruising.
Maximizing the benefits of Botox goes beyond merely avoiding certain activities or exercises. It involves a holistic approach that includes proper post-care. For instance, patients should avoid sun exposure, especially during outdoor activities, for the first 24 hours post-Botox to prevent migration of the treatment. Also, keeping the head upright for four hours and avoiding bending or lying down soon after Botox injections is crucial to ensure the treatment’s efficacy.
Maintaining hydration is critical after Botox, as it supports optimal skin condition and can enhance the treatment’s effects by contributing to healthier skin and plumping up the skin via hyaluronic acid. Moreover, to minimize risks such as increased bruising and to ensure optimal Botox results, it’s advised to avoid alcohol consumption, engage in gentle facial exercises, and not apply physical pressure to the treated area.
Additionally, applying a cold compress and sleeping with the head elevated can help minimize bruising and swelling post-treatment. All of these steps contribute to the overall success of your Botox treatment and can help ensure that you enjoy the benefits for as long as possible.
Navigating the post-treatment period after Botox can be a challenge, but with proper guidance and a bit of patience, it’s entirely manageable. From understanding what Botox is and how it works, to knowing the ideal wait time before resuming exercise after botox and what exercises are safe to perform, this guide has covered all the essentials. We’ve also discussed the importance of recognizing and managing post-Botox exercise symptoms, keeping your skin happy, and maximizing the benefits of Botox with proper post-care.
Remember, the key to enjoying the full benefits of your Botox treatment lies in the balance between maintaining an active lifestyle and giving your body the rest it needs post-treatment. With these tips in mind, you can ensure that your journey to a younger-looking, more radiant self is a safe and successful one.
Wait for at least 24 hours after your Botox treatment before engaging in strenuous exercise. This allows the Botox to settle into place and minimizes the risk of it moving to unintended areas.
To avoid compromising the effects of Botox, it's best to refrain from excessive sweating and hot environments for at least 24 hours after the injection. This can help prevent migration and maintain the desired outcome of the treatment.
To ensure the best results after Botox, avoid strenuous exercise for 24 hours, keep upright for 4 hours, avoid tight headwear, and reduce alcohol consumption or blood-thinning medication. These measures can help prevent complications and optimize the effectiveness of the treatment.
While there is a possibility of a slight chance of Botox migration within the first 24 hours, the risk is low and can be minimized by avoiding activities that involve bending over repeatedly. It's important to seek guidance from an experienced physician to ensure a safe procedure.
No, there is no correlation between exercise and Botox wearing off faster. It is safe to exercise regularly after Botox treatments.
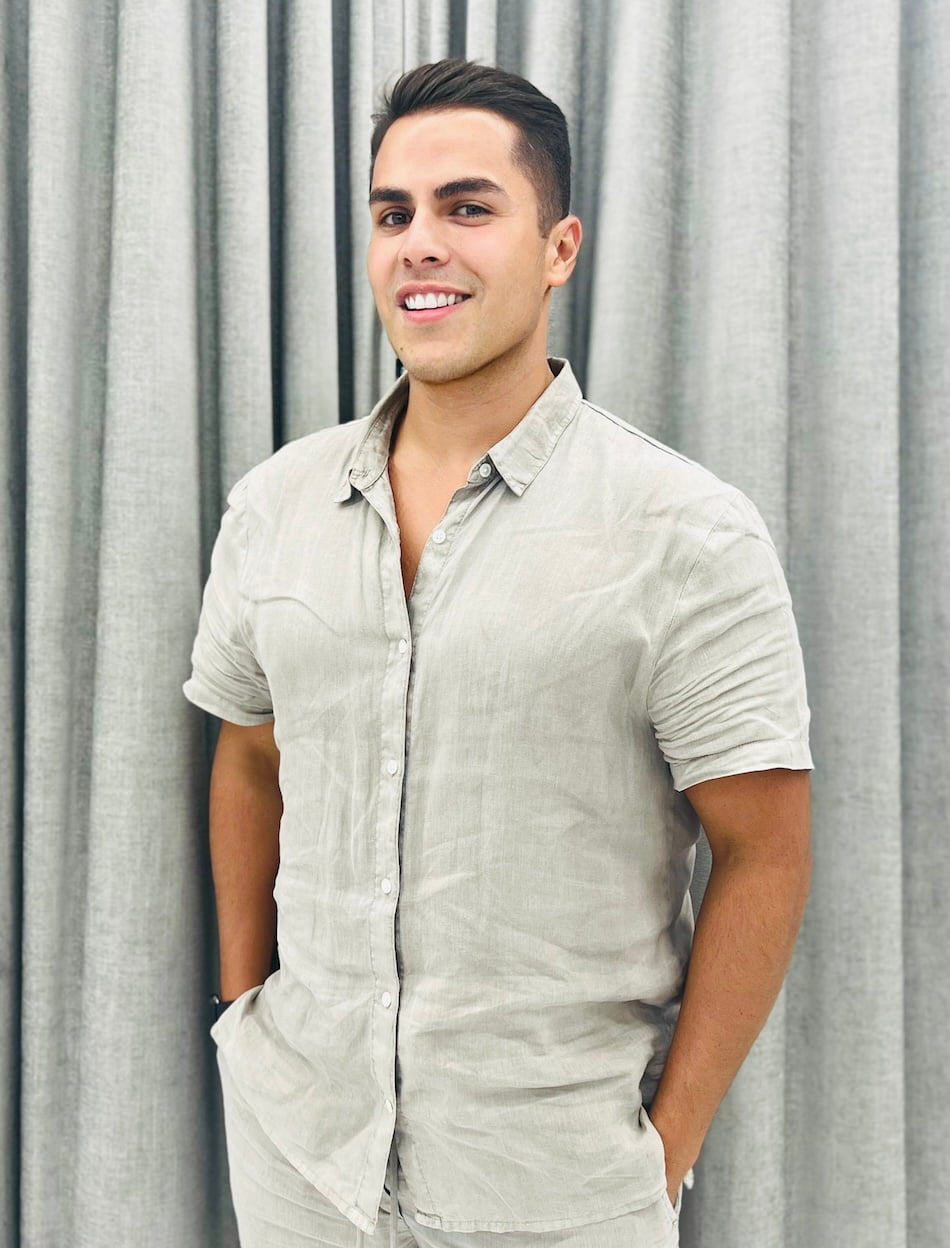
Dr. Alonso Martin is a renowned physician at the intersection of science, beauty, and longevity. Beginning his career at UCLA as a neuroscientist studying antioxidants' effects on longevity, Dr. Martin now leads AM Beauty & Wellness Medspa in Miami, specializing in the latest non-invasive facial and body rejuvenation techniques. His expertise spans cosmetic dermatology, focusing on injectable neuromodulators like Botox, Daxxify, Dysport, and Xeomin, alongside an array of fillers including RHA, Juvederm, and Sculptra, to name a few. He is also adept in natural skin rejuvenation through PRF (Platelet-Rich Fibrin), stimulating collagen production and mitigating signs of aging.
Further enhancing his practice's offerings, Dr. Martin utilizes Emsculpt NEO technology for muscle growth, tissue lifting, and fat elimination—techniques favored by NFL athletes and celebrities for strength and longevity. He passionately advocates for strengthening the body and optimizing its function as an anti-aging solution, incorporating peptide therapy to support overall wellness.
Dr. Martin trained at the University of California, Irvine Hospital in family medicine, where he treated patients of all ages with obesity, diabetes, thyroid & hormone disorders, high blood pressure, age-related diseases, chronic pain, and autoimmune conditions. With prestigious nominations like Resident of the Year at UCLA, he holds an M.D. from Michigan State University and a B.Sc. in Neuroscience from UCLA. Licensed in both Florida and California, Dr. Martin's credentials underscore his commitment to enhancing patient well-being through advanced medical practices.
If you have any questions or would like to schedule an appointment, contact AM Beauty & Wellness today by calling (305) 877-5084.
Schedule Your Consultation Today
The future looks brighter when you feel better. Dr. Alonso Martin and his team want to give you the joy of a longer, healthier life. Schedule your consultation today to learn how the right blend of anti-aging and nutrional intervention can help you improve your quality of life for years to come.
1060 Alton Rd, Miami Beach, FL 33139
Book directly online by following these easy steps
Or fill out this form to receive more information